Undocumented Domestic Workers and Coronavirus Disease 2019: A Qualitative Study on the Impact of Preventive Measures
- 1Department of Primary and Community Care, Radboud University Medical Centre, Nijmegen, Netherlands
- 2Pharos, Dutch Centre of Expertise on Health Disparities, Utrecht, Netherlands
- 3Runomi Radboud University Network on Migrant Inclusion, Nijmegen, Netherlands
- 4Department of Public and Occupational Health, Amsterdam Public Health Research Institute, Amsterdam University Medical Centre, University of Amsterdam, Amsterdam, Netherlands
- 5Faculty of Law, Centre for Migration Law, Radboud University, Nijmegen, Netherlands
- 6Stichting Fairwork, Amsterdam, Netherlands
This article describes the impact of coronavirus disease 2019 (COVID-19) preventive measures on the undocumented migrant domestic workers in the Netherlands. Undocumented migrants (UDMs) are likely to experience inequalities due to the COVID-19 pandemic. They rely on the informal market for work and housing and are usually not entitled to a healthcare insurance. However, they are not represented in the COVID-19 registrations or surveys. In order to advise the policymakers and healthcare professionals on how to tailor the preventive activities in handling a pandemic, including vaccination strategy, to the needs of this group, an insight into their experiences is needed. In our qualitative study, two focus group discussions were held with 14 UDMs, recruited through a snowball technique. The UDMs perceived the COVID-19 as a threat. Their precarious position affected their perceived vulnerability, which motivated them to seek information on and comply with preventive measures and testing. However, structural barriers decreased their self-efficacy and opportunity to comply. The COVID-19 measures impacted the lives of UDMs on essential domains, resulting in job, food, and housing insecurity, and increased barriers in access to healthcare. An intersectoral approach addressing health communication, access to healthcare, and social support, as well as legal rights for safe employment, is needed to alleviate the impact of the measures on UDMs.
Introduction
Undocumented migrants (UDMs), i.e., migrants residing in a host country without a lawful residence, are acknowledged as one of the most vulnerable groups who suffered from the coronavirus disease 2019 (COVID-19) pandemic (Bhopal R., 2020; Bhopal R. S., 2020; Shaaban et al., 2020), due to their disadvantaged working and living circumstances (Quinn and Kumar, 2014; Madhav et al., 2018; Hayward et al., 2021). In Europe, the number of UDMs is estimated between 3.9 and 4.8 million (Pew Research Center, 2019), while in the Netherlands, about 23,000–58,000, an approximate 0.3% of the Dutch population (Van der Heijden et al., 2020). In the Netherlands, UDMs are not entitled to work, nor rent a house. Informal, domestic work is one of the main sectors where UDMs find an employment (Parrennas et al., 2018), also in the Netherlands (Berntsen et al., 2021), and irrespective of applicable human rights, they face specific challenges and vulnerabilities (see Box 1).
Box 1. Rights and Living conditions of undocumented migrants (UDMS) domestic workers in the Netherlands.
The UDMs in the Netherlands are excluded from most of the government facilities through the Linking Act, linking their residence status to access social welfare arrangements, including social housing. Thus, UDMs rely on informal housing.
They do remain eligible for healthcare but have to pay the costs themselves as they are excluded from health insurance and education up to the age of 18 years old.
The Netherlands has not ratified the International Labour Organisation (ILO) Domestic Workers Convention No. 189, recognizing that it is desirable to offer them decent working conditions. In the Netherlands, their work includes cleaning, babysitting, elderly care, gardening, et cetera. They are not insured but they are entitled to:
- Minimum wage (EURO 9.96 per hour for workers over 21 years of age)
- Four weeks of paid leave annually and,
- in case of illness, 6 weeks of continuous pay.
Employers, including private households, risk administrative fines when employing UDMs.
The UDMs do not risk a fine, but deportation.
The opportunities to apply for legal residence as a migrant worker with an employer sponsor are limited and are mainly open only to those performing (highly) qualified jobs.
Having to rely on the informal market makes the UDMs subject to low wages, crowded housing, and general exploitation (Parrennas et al., 2018; Varga, 2020), as well as elevated physical and psychological stress (Schoevers et al., 2009; Teunissen et al., 2014a,b; Andersson et al., 2018). This increases their risk for COVID-19 exposure (Burton-Jeangros et al., 2020; Devillanova et al., 2020; Mia and Griffiths, 2020) and severe disease (Fiorini et al., 2020).
Unfortunately, preventive communication on protective measures is mostly in national languages and often designed according to social and cultural norms that migrants may not relate to (Fiorini et al., 2020) (see Box 2 for the protective measures in the Netherlands).
Box 2. COVID-19 preventive measures in the Netherlands at the time of the study (November 2020)a.
General preventive measures applicable throughout the pandemic:
➢ Keep a distance of 1.5 meters between you and other persons;
➢ Disinfect your hands regularly;
➢ Sneeze and cough not in your hand but in the crook of your elbow;
➢ Use a facemask in public transport and in shops; and
➢ Refrain from personal contact when having symptoms of a cold and get yourself tested.
November 2020 – second wave:
➢ Maximum group size allowed to gather outside of 2 (other than family members);
➢ Maximum number of house guests of 4, later 2;
➢ All restaurants, schools, non-essential stores, and public buildings closed; and
➢ Working and staying at home as much as possible.
aAvailable online at: https://www.rijksoverheid.nl/actueel/nieuws/2020/11/03/tijdelijke-verzwaring-van-de-gedeeltelijke-lockdown.
Furthermore, access to care for UDMs is limited. The UDMs are not eligible for healthcare insurance, and, although in the Netherlands, UDMs have a right to access all the medically necessary care (Smith and LeVoy, 2017), this access is limited due to legal, administrative, linguistic, social, and cultural barriers, a lack of trust in the (healthcare) system, fear of losing work or, ultimately, deportation (Schoevers et al., 2010; Terminski, 2013; Woodward et al., 2014; Fiorini et al., 2020; Varga, 2020).
Besides the immediate negative influence of COVID-19 on the health of this vulnerable population, there is substantial “collateral damage” (Cénat et al., 2020) due to the cancellation of less urgent care and the impact of government-imposed preventive measures on working and living conditions. As such, a pandemic adds to the burden of “structural violence” (Farmer et al., 2006) to the marginalized groups experience and can contribute to the deepening of health inequalities.
In order to spread the burden of the pandemic, countries should assess which members of society are most vulnerable and should fairly support those at the highest risk” (Lancet, 2020). However, due to the nature of their legal status and a general lack of health-related data by migrant status or ethnicity (Shaaban et al., 2020), UDMs are not represented in the official COVID-19 registrations in the Netherlands, nor surveys on uptake and impact of preventive measures. This brings about a paucity of information on how to mitigate the specific effects of the COVID-19 pandemic for UDMs in the Netherlands and to mitigate the deepening of health inequalities and social injustice.
In order to advise the policymakers and healthcare professionals on tailoring the communication and activities related to the handling of a pandemic, including vaccination strategies to the needs of UDMs, an insight into the experiences of this marginalized group is needed. This qualitative study explores the impact of COVID-19 preventive measures on the lives of UDMs domestic workers in the Netherlands.
Materials and Methods
Design
For this qualitative study, we held two focus group discussions (FGDs) with UDMs. This study is part of two larger studies: (a) “Ethnicity and COVID-19: epidemiology and control measures” and (b) “Migrants in the frontline”. Ethical approval has been provided by the Radboud University Ethics Assessment Committee Law and Management (EACLM Ref No: 2021.04).
Research Population
Persons were eligible for participation if they spoke English or Dutch and were migrant domestic workers without a legal staying permit for the Netherlands. We approached trusted networks of migrant organizations throughout the Netherlands and used snowball techniques, whereby the confirmed participants were asked to introduce other potential participants, who were subsequently contacted.
Data Collection and Analysis
We developed a topic list for the FGDs based on literature and expert opinion. It contained questions on knowledge, uptake, and impact of COVID-19 preventive measures in relation to working and living circumstances and access to healthcare.
At the time of data collection (November 2020), the Netherlands was in partial lockdown and the FGDs had to be performed online using a video conferencing software. We chose ZOOM (Zoom Cloud Meetings for Windows) as most participants shared they had prior experience using this platform, e.g., for online church meetings. Two authors (MT and NS) facilitated the FGD.
Focused group discussions (FGDs) with a duration of ~2 h each were audio-recorded and transcribed. We analyzed the transcripts thematically by using a qualitative data analysis software MAXQDA (MAXQDA VERBI Software GmbH Berlin, Germany). We developed a coding system including codes on accessing the information on preventive measures, factors affecting uptake of preventive measures, and impact of the preventive measures and pandemic. Codes on the uptake of measures were informed by Protection Motivation Theory, which is a model used to predict the behavior, which is specifically in response to the health threats that can be useful in understanding people's behavioral response to the COVID-19 control measures (Norman et al., 2015) (see Box 3).
Box 3. The protection motivation theory.
The protection motivation theory is a model used to predict a behavior that is specifically in response to health threats that can be useful in understanding the behavioral response of the people to the COVID-19 control measures.
Protection motivation (i.e., intention to perform a recommended behavior) resulted from two appraisal processes, threat appraisal and coping appraisal, and is a positive function of a perceived vulnerability to the health threat, perceived severity of the health threat, perceived response efficacy, and self-efficacy (Norman et al., 2015).
Two researchers have independently read and coded the transcripts. They identified and discussed the themes and subthemes until an agreement was reached, which were subsequently added to the coding system (e.g., criminalization).
As the UDMs population in the Netherlands is small and we wish to ensure anonymity, we do not refer to the characteristics of the respondents in relation to the reported quotes. Instead, we refer to the position of the quote in the transcript.
Results
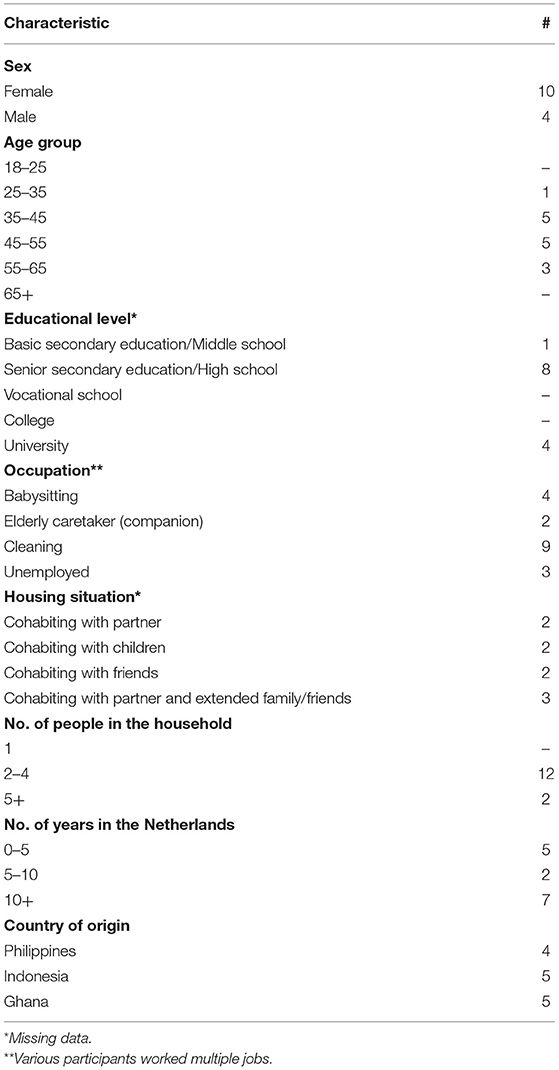
Fourteen UDMs participated in the FGD. The majority of participants (N = 12) had finished secondary education or higher, but all the participants performed low classified jobs as babysitters or cleaners. Three participants were currently unemployed. The majority (N = 9) resided in the Netherlands for 5 ≤ years. All participants had frequent, daily, or weekly contact with people in their country of origin (see Table 1).
Uptake of Preventive Measures
UDMs Feel Vulnerable Due to Their Precarious Position
Participants indicated that they knew the health risks of the coronavirus. They were aware that doing domestic work means coming into close contact with household members and moving between various households, which places them at risk of both contracting and spreading the coronavirus (#01). They mentioned the employers asking them to come to work during, or shortly after an infection in their household, without previously informing them about it (#02).
#01 “We are really at risk in our everyday lives. We're frontliners in our own way because we go out every day to... help the household that we work for, help the parents with their kids who go to school, who also get in contact with other people - a lot of people. Sometimes we take public transport to go to work. So really, you could say that we are very high risk in terms of contracting the corona disease. Because of the nature of our work.” (20201101FGD4_transcript: 15 - 17)
#02“And me and my partner we were living in with our employer. They had a ski holiday and they didn't tell us that they have experienced symptoms of corona. They all got tested and some of their group were positive, but didn't let us know…” (20201101FGD4_transcript: 21 - 21).
UDMs Have High Information Needs
Participants had confidence in the efficacy of control measures (#03, #04). And, as they perceived a high threat of becoming infected, they felt they were required to be well-informed of the preventive measures (#05), particularly, on the appropriate quarantining time after a positive test result in the household.
Participants got their information through official news channels and social media (#06). Those who experienced a language barrier used websites for ex-pats that shared the news in English or depended on community leaders and people in their network to translate and communicate the information to them, mostly through social media (#07). This caused a slight delay in access to information (#08).
#03 “…Keeping 1.5 meters, is really good. Because when you protect yourself, it's better. When you protect yourself, like you use the hand sanitizer, you wash your hands, stay away from public places... It's good…” (20201126FGD5_transcript: 86 - 88)
#04 “First washing your hands and also keeping the distance for me it is not that disturbing. Why? I talked to one of my friends in Ghana and he is a doctor and he said something. He said that corona has taken away cholera from there. Because everyone is washing his or her hands and no handshaking. That is good.” (20201126FGD5_transcript: 115 - 115)
#05 “I think the rules are pretty obvious and we would see them also online. Working around a lot of people, we want to know the rules first. So we know we don't break the rules. Second, that the people around us also don't break the rules, then we are also safe.” (20201101FGD4_transcript: 73 - 73)
#06 “Normally, people here when we get something, we share it by WhatsApp. So when I get something I also send someone. So that's where I get the information. And sometimes when I get something I don't understand, I have a friend from Holland who I invite here and I ask: “what do you think about it; what do they say?” Then he can explain to me…” (20201126FGD5_transcript, Pos. 129)
#07 “There are some Ghanaian leaders who always come out with the news: “this is what the Prime Minister Rutte has said”; So we hear a lot on social media.” (20201126FGD5_transcript: 121 - 123)
#08 “If you translate it for us we would be very very grateful. So that we know the rules very well and fast and we must not wait for one or two days. Maybe some expats translate it, but some of the expats do not know Dutch very well, not as good as the Dutch people.” (20201101FGD4_transcript: 148 - 148).
Structural Barriers Decrease Compliance to the Preventive Measures
The participants indicated they want to live by the measures, even if it requires the behavior that is contrary to what they are (culturally) accustomed to (#09). They were early adopters of the use of preventive face-masks, especially when relying on public transport, but reported feeling stressed about forgetting to carry a facemask and being fined as a consequence (#10, #11). As mentioned above, however, participants shared several examples of not being able to comply with the preventive measures due to their precarious position as UDMs. They indicated that the uptake of testing by UDMs is affected by several barriers.
At the beginning of the pandemic, there was limited availability of tests for the general population and accessibility remained an issue once testing became available (e.g., long waiting times for the telephone service). In combination with limited accessibility of General Practices due to practices being closed for physical visits, this posed a barrier for participants who were concerned about their health.
Even at the moment of the FGDs, in November 2020, not all participants knew how to get tested. The language was a barrier, as was their lack of legal documents. The participants indicated that UDMs could be reluctant in identifying themselves, fearing legal consequences, or were hindered because they lacked the necessary national identification number (BSN) and were unaware of the options to register for testing without it (#12).
Lastly, upon suffering from COVID-19, undocumented migrants may face difficulties in isolating themselves as a consequence of their living situation, i.e., many participants rent a room in a house shared with a number of other undocumented migrants.
#09 “For example, in my culture if you meet somebody you have to shake hands. But with the person you are shaking hands, you don't know where he is coming from. Another person is coming from wc and he or she has not washed his or her hands..” (20201126FGD5_transcript: 115 - 115)
#10 “The mask... I don't like it. Because if I put the mask in about three or four minutes I cough., And within one second I am yawning. So I don't feel comfortable with it. All the time I forget it. If you forget it you can't enter the metro and the public transport. So always it gives me stress.” (20201126FGD5_transcript: 78 - 88)
#11 “If because of corona you get a bill for maybe 95 euros it's very difficult. If you don't have the document and also you don't know how to pay it's going to get you into trouble.” (20201126FGD5_transcript: 195 - 197)
#12 “People we know (..) called the municipal health service and told that they wanted to get tested, but were asked for their national identification number (BSN) but they don't have BSN (..)Then she (the municipal health service employee) told ‘you have nothing to worry about'. That is one of the things that we are also very grateful for, that at least this person (…) was very helpful and was very reassuring. But it will not be the case for everyone..” (20201101FGD4_transcript: 97 - 100).
COVID-19 Measures Increase Job, Food, and Housing Insecurity
The COVID-19 measures impacted the lives of the participants in multiple aspects. They shared feeling of being worried and stressed because they fear, or have experienced, loss of employment with food and housing insecurity as a consequence (#13). Many participants experienced a loss of income. Some of them were pushed to leave a household because they experienced mistreatment, e.g., being forced to come to work despite a case of COVID-19 in the household (#14). Others were asked to stay away, either temporarily or permanently (#15).
Only one participant continued to receive a part of their wages. The loss of income poses major challenges as UDMs do not have access to financial support systems that the government has put in place (#16). They mentioned examples of solidarity among UDMs and support from others to survive (#17), such as help in navigating the health care system, support with food, and financial assistance, either by providing this or directing their members to organizations where these are available (#18). However, these voluntary initiatives also come to the end of their resources eventually (#19).
#13 “The past week, there had been some rumors that there might be a lockdown. It was quite worrisome, because we don't know what would be the response of our other employers. Because we work with several households. … if our employers still want us to come? And if they don't let us come to work, will they at least still be paying us?” (20201101FGD4_transcript: 6 - 6)
#14 “They did not let us know about the infection (–see quote above). So it was very difficult. In the end we decided to leave that work. So we lost 80% of our work and then on top of that we had to find a new place to live in.” (20201101FGD4_transcript: 21 - 21)
#15 “Because you have to go to somebody's place to work and everybody is afraid. They said ‘you have to take off some time'. But now still, nobody is calling me to come back. So that's the problem.” (20201126FGD5_transcript: 45 - 47)
#16 “I lost my job, and don't know how to survive. Undocumented people sometimes don't pay rent, but pay a little to help them. If you are losing your job, what can you do? This became a problem for a number of undocumented. You hear that the government is helping those who have the paper. Or have the number. But those who don't have that, what can they do?” (20201126FGD5_transcript: 70 - 70)
#17 “…So it's difficult for them to survive. That's why we are thinking that if our members don't have a house or money we (self-organization) need to find a shelter for them.” (20201101FGD4_transcript: 19 - 19)
#18 “If we learn that there is a foundation that gives €100 to women, during the pandemic, than we (self-organization) tell our female members: ‘call or email them so that we can schedule a meeting to know more about the assistance that they are giving right now.' That is the resilience in the community effort. People helping people so that we can at least cope in the situation.” (20201101FGD4_transcript: 36 - 36)
#19 “You see, living here without work it's not easy. When I go to the organization, I can get food to eat, but to get a place where to sleep and to get peace of mind it's another issue. So it came to a time then she (the landlord) could not help anymore. Because she had to pay the water bill. And you cannot live in a house without taking a shower.(..) You know, Holland here, everything is about money.. So it was coming to a time that she was fed up. It's a little bit hard.” (20201126FGD5_transcript: 105 - 109).
Increased Racial Discrimination
Some participants with a Filipino or Indonesian background reported experiencing an anti-Asian racism and criminalization as a consequence of wearing a facemask (#20, #21).
#20 “... Sometimes I have an impression that you are just applying the distance rules to me because of my skin color. Because you are white and you are not wearing a mask. You are making me more susceptible to contracting corona. I'm wearing a mask and people would look at me like I am the whole walking virus, because I am wearing a mask but they are not. That was just my impression. And that is something that really annoys me and makes me insecure as well.” (20201101FGD4_transcript: 83 - 83)
#21 “One of our members was using the mask outside...at eight o'clock in the morning. Suddenly the police stopped him and asked his ID. Because he was wearing a mask. And in that area there was a house burglary. So when the police saw somebody with a mask, they recognized him as somebody doing the burglary. That is very weird you know. We try to stop corona; we use the mask, and the police asks because we are wearing mask. That is really weird.” (20201101FGD4_transcript: 85 - 85).
Increased Barriers in Accessing Healthcare
The participants experienced barriers to healthcare. In accessing care, UDMs depend on support by self-organizations, especially when they face a language barrier. Most of our participants were members of such organizations and, therefore, knew how to access this support system. Some offered such support themselves. However, they indicated that not every UDM knows where to find support.
The participants, furthermore, indicated that the organizations who function as gateways to accessing healthcare [e.g., General Practitioner (GP) practices accessible for UDMs] were unavailable for visits during the beginning of the pandemic, and until now, some practices only see a limited number of patients a day to avoid crowding in waiting rooms, etc. (#22). Furthermore, non-COVID care has been postponed, affecting the UDMs in need of treatment (#23).
#22 “I think they have a limit at the Kruispost (a voluntary healthcare organization for UDMs) of only 15 people that can be assisted. And a maximum of three inside the waiting room. If you come later you are not able to get a slot. Unlike before, you know, they served as many people as they could in the time. So it's a bit sad if you don't get tested because the time is up. Uh, if you don't get checked.” (20201101FGD4_transcript: 135 - 135)
#23 “I'm supposed to have this operation, but due to the corona they have been postponing I have to wait for three months or more. And I'm in pain. it's given me a headache, really. I'm stressed out for this since, because I'm supposed to do the operation but I cannot go to the hospital now. I have to wait. The doctor told me that they have more than fifty patients waiting because of the corona. So the corona has caused a lot of pains.” (20201126FGD5_transcript: 39 - 39).
Discussion
Main Results
The undocumented migrant domestic workers in this qualitative study perceived the coronavirus as a threat and regarded the preventive measures as effective. Their precarious position increased their perceived vulnerability, which motivated them to seek information on preventive measures and testing and to comply with the measures. However, they experienced a delay in access to information and structural barriers decreased their self-efficacy to comply. The COVID-19 measures impacted their lives on essential domains, as they lead to job, food, and housing insecurity and increased barriers in access to healthcare. Individual community members, non-government organizations (NGOs), and migrant organizations provided support, but participants felt these were reaching their limits.
Comparison With Literature
To the best of our knowledge, this is the first study on the uptake of COVID-19 preventive measures amongst UDMs. Our findings with regards to the knowledge and motivation to comply with preventive measures are comparable with other studies amongst the migrant populations in the Netherlands (Van Loenen et al., 2020; Torensma et al., 2021). The reported impact of the COVID-19 measures and larger pandemic is similar to the findings by Spiritus, who found an increase in daily life stressors among the refugees and other migrants in Europe (Spiritus-Beerden et al., 2021).
Reported difficulties in accessing information and complying with measures are colored by the challenging living and working conditions of UDMs. The UDMs' precarious circumstances are well-known from previous studies in the Netherlands and elsewhere (Schoevers et al., 2009, 2010; Woodward et al., 2014) and have been observed in the few other studies on the impact of COVID-19 on UDMs elsewhere (Schoevers et al., 2009; Burton-Jeangros et al., 2020; Devillanova et al., 2020; Fiorini et al., 2020; Mia and Griffiths, 2020; Varga, 2020). In turn, non-compliance poses a health risk as access to healthcare is hampered for UDMs, especially for those who are not aligned with NGO or migrant organizations (Schoevers et al., 2010). And, similar to our findings, studies on the use of healthcare during the first pandemic wave registered a decreased access to healthcare (Van Weert, 2020).
These findings confirm the structural societal disadvantage that the UDMs face, characterized as structural violence—the “avoidable impairment of fundamental human needs, which lowers the actual degree to which someone is able to meet his needs and to reach his full potential.” (Farmer et al., 2006)—that is exacerbated by the COVID-19 pandemic and, as such, may contribute to the deepening of health inequalities. To relieve this burden and to achieve equitable chances for good health is beyond the individual medical domain. It requires structural measures, an intersectoral approach simultaneously targeting different domains of insecurity that are parallel to actions on the underpinning of social and political determinants of these vulnerabilities (Jackson et al., 2021) (see Box 4).
Box 4. Recommendations.
Our results show the need for improving the reach and effectiveness of governmental and public health policies for the group of UDMs. In addition, they indicate multiple opportunities for improvement. We specifically recommend to:
1. Publish the information on preventive measures immediately and widely, in different languages, in easy-to-understand terms (e.g., using visual images), and tailored to the specific situation of UDMs. For instance, addressing the question of how to access testing or vaccination when one does not possess the national identification number (BSN);
2. Inform UDMS about their rights regarding their employment and access to healthcare;
3. Inform employers of their duties to conduct good employership, also regarding UDMs;
4. Tailor-fit the outreach strategies of public health services for improving participation in testing and vaccination to the needs of the UDMs, by involving local migrant support organizations in the development and implementation of these strategies;
5. Involve volunteers to support UDMs in accessing healthcare and handling remote consultations;
6. (for healthcare professionals) Involve professional interpreters, also in remote consultations;
7. Admit UDMs to access homeless shelters, at least in the coming year, as it is likely that the loss of housing will continue to be a problem in UDMS especially when they will not be able to return to their country of origin; and
8. Admit UDMs to existing regulations that compensate for financial problems due to the loss of jobs as a result of the pandemic.
One such determinant is the lack of access to information.
Health communication is a key and a necessary factor in saving lives during crises like the COVID-19 pandemic (Finset et al., 2020). Providing UDMs with timely and accessible information to protect themselves from the COVID-19 infection, as well as to protect their rights as workers, right to housing, and healthcare can aid their position.
Understandable and culturally acceptable information from a trusted source like religious or community leaders can help establish an equitable access to preventive measures and healthcare (Finset et al., 2020; Kulich et al., 2021; Thomas et al., 2021). The Information and Communication Technology (ICT) can play a role particularly in reaching migrants with limited health literacy (Ahmed, 2018).
Strengths and Weaknesses
Thanks to the collaboration of the key persons from UDM communities, we were able to include this so-called “hard-to-reach” group (Van den Muijsenbergh et al., 2016), even in an online FGD. As a consequence of our recruitment strategy, participants were mostly, if not all, active members of their respective communities, which may mean we included more highly educated and more vocal representatives. Because of this, they could advocate well for their communities and share the experiences of members to their respective organizations. On the other hand, the fact that this is not a representative sample may have obscured the (first-hand) experiences of those on the very margins of society or from those which were not included in the migrant groups. English or Dutch, the languages used during the FGD are not the mother tongue of all participants, which could limit their possibilities to express themselves.
Conclusion
The precariousn position of the Undocumented migrants motivates them to seek information and to comply with preventive measures and testing. Structural barriers decrease their self-efficacy and opportunity to comply. Concurrently, the negative impact of preventive COVID-19 measures on the living circumstances and access to healthcare of UDMs exemplifies the “structural violence” they experience. An integrated intersectoral approach, addressing access to healthcare and social support is needed to alleviate this impact.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Radboud University Ethics Assessment Committee Law and Management (EACLM Ref No: 2021.04). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
MM, KS, and TL initiated the study and wrote the research proposal. MT and NS did the fieldwork. All authors were involved in analyzing the data and commenting on the drafts of the manuscript that MM wrote. All authors contributed to the article and approved the submitted version.
Funding
This study had received funding from the ZonMw, The Netherlands Organization for Health Research and Development.
Conflict of Interest
MM was employed by Pharos. NS was employed by Stichting Fairwork.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We would like to thank all participants for the FGDs.
References
Ahmed, R. (2018). Challenges of migration and culture in a public health communication context. J. Public Health Res. 7:1508. doi: 10.4081/jphr.2018.1508
Andersson, L. M. C., Hjern, A., and Ascher, H. (2018). Undocumented adult migrants in Sweden: mental health and associated factors. BMC Public Health 18, 1–9. doi: 10.1186/s12889-018-6294-8
Berntsen, L., de Lange, T., and Rijken, C. R. J. J. (2021). (In Dutch) Migranten zonder verblijfsvergunning: hun rechten en sociaaleconomische positie in Nederland. (Migrants without staying permit: their rights and socioeconomic position in the Netherlands), AUP Amsterdam.
Bhopal, R. (2020). Covid-19: undocumented migrants are probably at greatest risk. BMJ 369, m1673. doi: 10.1136/bmj.m1673
Bhopal, R. S. (2020). COVID-19: Immense necessity and challenges in meeting the needs of minorities, especially asylum seekers and undocumented migrants. Public Health 182, 161. doi: 10.1016/j.puhe.2020.04.010
Burton-Jeangros, C., Duvoisin, A., Lachat, S., Consoli, L., Fakhoury, J., and Jackson, Y. (2020). The Impact of the Covid-19 pandemic and the lockdown on the health and living conditions of undocumented migrants and migrants undergoing legal status regularization. Front. Public Health 8, 596887. doi: 10.3389/fpubh.2020.596887
Cénat, J. M., Dalexis, R. D., Kokou-Kpolou, C. K., Mukunzi, J. N., and Rousseau, C. (2020). Social inequalities and collateral damages of the COVID-19 pandemic: when basic needs challenge mental health care. Int. J. Public Health 65, 717–718. doi: 10.1007/s00038-020-01426-y
Devillanova, C., Colombo, C., Garofolo, P., and Spada, A. (2020). Health care for undocumented immigrants during the early phase of the Covid-19 pandemic in Lombardy, Italy. Eur. J. Public Health 30, 1186–1188. doi: 10.1093/eurpub/ckaa205
Farmer, P. E., Nizeye, B., Stulac, S., and Keshavjee, S. (2006). Structural violence and clinical medicine. PLoS Med. 3, e449. doi: 10.1371/journal.pmed.0030449
Finset, A., Bosworth, H., Butow, P., Gulbrandsen, P., Hulsman, R. L., Pieterse, A. H., et al. (2020). Effective health communication–a key factor in fighting the COVID-19 pandemic. Patient Educ. Couns. 103, 873. doi: 10.1016/j.pec.2020.03.027
Fiorini, G., Rigamonti, A. E., Galanopoulos, C., Adamoli, M., Ciriaco, E., Franchi, M., et al. (2020). Undocumented migrants during the COVID-19 pandemic: socio-economic determinants, clinical features and pharmacological treatment. J. Public Health Res. 9, 1852. doi: 10.4081/jphr.2020.1852
Hayward, S. E., Deal, A., Cheng, C., Crawshaw, A., Orcutt, M., Vandrevala, T. F., et al. (2021). Clinical outcomes and risk factors for COVID-19 among migrant populations in high-income countries: a systematic review. J. Migr. Health 2021, 100041. doi: 10.1016/j.jmh.2021.100041
Jackson, Y., Sibourd-Baudry, A., Regard, S., and Petrucci, R. (2021). Vulnerable populations and COVID-19 : need for innovation and cooperation to address health and social needs. Rev. Med. Suisse. 17, 243–247.
Kulich, S. J., Komisarof, A., Smith, L. R., and Cushner, K. (2021). Re-examining intercultural research and relations in the COVID pandemic. Int. J. Intercul. Relat. 80, A1–6. doi: 10.1016/j.ijintrel.2020.12.003
Lancet, T. (2020). Redefining vulnerability in the era of COVID-19. Lancet 395, 1089. doi: 10.1016/S0140-6736(20)30757-1
Madhav, N., Oppenheim, B., Gallivan, M., Mulembakani, P., Rubin, E., Wolfe, N., et al. (2018). Pandemics: risks, impacts, and mitigation in: Jamison D TH et al. (edit). Disease control priorities: improving health and reducing poverty. Disease Control Priorities (third edition), Vol. 9 (Washington, DC: World Bank). chapter 17 (315 – 47).
Mia, M. A., and Griffiths, M. D. (2020). Letter to the Editor: the economic and mental health costs of COVID-19 to immigrants. J. Psychiatr. Res. 128, 23. doi: 10.1016/j.jpsychires.2020.06.003
Norman, P., Boer, H., and Seydel, E. R. (2015). “Protection motivation theory,” in Predicting Health Behaviour: Research and Practice With Social Cognition Models, editors M. Conner and P. Norman (Open University Press), 81–126.
Parrennas, R. S., Silvey, R., Hwang Rice, M. C., and Areum Choi, C. (2018). Serial labor migration: precarity and itinerancy among Filipino and Indonesian domestic workers. Int. Migr. Rev. 53, 1230–1258. doi: 10.1177/0197918318804769
Pew Research Center (2019). Europe's Unauthorized Immigrant Population Peaks in 2016, Then Levels Off . Washington, DC.
Quinn, S. C., and Kumar, S. (2014). Health inequalities and infectious disease epidemics: a challenge for global health security. Biosec. Bioterr. 12, 263–273. doi: 10.1089/bsp.2014.0032
Schoevers, M. A., Loeffen, M. J., van den Muijsenbergh, M., and Lagro-Janssen, A. L. (2010). Health care utilisation and problems in accessing health care of female undocumented immigrants in the Netherlands. Int. J. Public Health 55, 421–428. doi: 10.1007/s00038-010-0151-6
Schoevers, M. A., van den Muijsenbergh, M., and Lagro-Janssen, A. L. (2009). Self-reported health problems of female undocumented immigrants. Top of the iceberg. Self-rated health and health problems of undocumented immigrant women in the Netherlands, a descriptive study. J. Public Health Policy 30, 409–422. doi: 10.1057/jphp.2009.32
Shaaban, A. N., Peleteiro, B., and Martins, M. R. O. (2020). The Writing's on the wall: on health inequalities, migrants, and coronavirus. Front. Public Health 8, 505. doi: 10.3389/fpubh.2020.00505
Smith, A. S., and LeVoy, M. (2017). City of Rights. Ensuring Health Care for Undocumented Residents. Brussels: Picum, 24p.
Spiritus-Beerden, E., Verelst, A., Devlieger, I., Langer Primdahl, N., Botelho Guedes, F., Chiarenza, A., et al. (2021). Mental Health of Refugees and Migrants during the COVID-19 pandemic: the role of experienced discrimination and daily stressors. Int. J. Environ. Res. Public Health 18, 6354. doi: 10.3390/ijerph18126354
Terminski, B. (2013). “Realizing the right to health of undocumented immigrants in Europe: legal and social challenges,” in Proceedings of the 13th World Congress on Public Health (Bologna: Monduzzi Ed), 1–12. Available online at: https://www.ssoar.info/ssoar/bitstream/handle/document/35974/ssoar-2013-terminski-Realizing_the_right_to_health.pdf?sequence=1 (accessed February 3, 2022).
Teunissen, E., Sherally, J., van den Muijsenbergh, M., Dowrick, C., van Weel-Baumgarten, E., and van Weel, C. (2014a). Mental health problems of undocumented migrants (UM) in the Netherlands: a qualitative exploration of help-seeking behaviour and experiences with primary care. BMJ Open 4, e005738. doi: 10.1136/bmjopen-2014-005738
Teunissen, E., van den Bosch, L., van Bavel, E., van den Driessen Mareeuw, F., van den Muijsenbergh, M., van Weel-Baumgarten, E., et al. (2014b). Mental health problems in undocumented and documented migrants: a survey study. Fam. Pract. 31, 571–577. doi: 10.1093/fampra/cmu038
Thomas, C. M., Osterholm, M. T., and Stauffer, W. M. (2021). Critical considerations for COVID-19 vaccination of refugees, immigrants, and migrants. Am. J. Trop. Med. Hyg. 104, 433. doi: 10.4269/ajtmh.20-1614
Torensma, M., Harting, J., Boateng, L., Agyemang, C., Lassooy Tekle, Y., Jacob, Y., et al. (2021). Contextual factors that shape uptake of COVID-19 preventive measures by persons of Ghanaian and Eritrean origin in The Netherlands: a focus group study. J. Migr. Health 4, 100070. doi: 10.1016/j.jmh.2021.100070
Van den Muijsenbergh, M., Teunissen, E., van Weel-Baumgarten, E., and van Weel, C. (2016). Giving voice to the voiceless. How to involve vulnerable migrants in healthcare research. Br. J. Gen. Pract. 66, 284–285. doi: 10.3399/bjgp16X685321
Van der Heijden, P. G. M., Cruyff, M. J. L. F., Engbersen, G. B. M., and van Gils, G. (2020). (In Dutch): Schattingen onrechtmatig in Nederland verblijvende vreemdelingen 2017-2018. (Estimates of illegally residing migrants in the Netherlands). Wetenschappelijk Onderzoek- en Documentatiecentrum (WODC). Available online at: https://repository.wodc.nl/handle/20.500.12832/3010 (accessed February 3, 2022).
Van Loenen, T., Denktaş, S., Merkelbach, I., and van den Muijsenbergh, M. (2020). (In Dutch) Kennis, naleving en gevolgen van de Corona gedragsmaatregelen voor sociaal kwetsbare groepen en mensen met een migratieachtergrond. (Knowledge, Compliance and impact of Corona behavior measures on socially vulnerable groups and people with migration background). Pharos/Radboudumc/EUR Utrecht.
Van Weert, H. (2020). After the first wave: What effects did the COVID-19 measures have on regular care and how can general practitioners respond to this? Eur. J. Gen. Pract. 26, 126–128. doi: 10.1080/13814788.2020.1798156
Varga, B. M. (2020). Access to healthcare services for the Roma and undocumented migrants in the EU in light of the COVID-19pandemic. Int. J. Roma Stud. 2, 4–27. doi: 10.17583/ijrs.2020.5952
Keywords: undocumented, migrants, COVID-19, preventive measures, structural violence
Citation: van den Muijsenbergh M, Torensma M, Skowronek N, de Lange T and Stronks K (2022) Undocumented Domestic Workers and Coronavirus Disease 2019: A Qualitative Study on the Impact of Preventive Measures. Front. Commun. 7:736148. doi: 10.3389/fcomm.2022.736148
Received: 13 July 2021; Accepted: 18 January 2022;
Published: 04 March 2022.
Edited by:
Satveer Kaur-Gill, Massey University, New ZealandReviewed by:
Ravindra Kumar Vemula, English and Foreign Languages University, IndiaAsha Rathina Pandi, Massey University, New Zealand
Md Mahbubur Rahman, Massey University, New Zealand
Copyright © 2022 van den Muijsenbergh, Torensma, Skowronek, de Lange and Stronks. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Maria van den Muijsenbergh, maria.vandenmuijsenbergh@radboudumc.nl
 Maria van den Muijsenbergh
Maria van den Muijsenbergh Marieke Torensma4
Marieke Torensma4