Abstract
The aim of this study was to examine whether therapeutic communication improves children’s comfort during venipuncture compared to standard communication. This study was registered in the Dutch trial register (NL8221), December 10, 2019. This single-blinded interventional study was carried out in an outpatient clinic of a tertiary hospital. Inclusion criteria were age between 5 and 18 years, use of topical anesthesia (EMLA) and sufficient understanding of the Dutch language. 105 children were included, 51 assigned to the standard communication group (SC group) and 54 patients to the therapeutic communication group (TC group). The primary outcome measure was self-reported pain based on the Faces Pain Scale Revised (FPS-R). Secondary outcome measures were observed pain (numeric rating scale (NRS)), self-reported/observed anxiety in child and parent (NRS), self-reported satisfaction in child, parent and medical personnel (NRS), and procedural time. No difference was found for self-reported pain. Self-reported and observed anxiety (by parents and medical personnel) was lower in the TC group (p-values ranged from p = 0.005 to p = 0.048). Procedural time was lower in the TC group (p = 0.011). Satisfaction level of medical personnel was higher in the TC group (p = 0.014).
Conclusion: TC during venipuncture did not result in lower self-reported pain. However, secondary outcomes (observed pain, anxiety and procedural time) were significantly improved in the TC group.
What is Known: • Medical procedures, especially needle related procedures, cause anxiety and fear in children and adults. • In adults communication techniques based on hypnosis are effective in reducing pain and anxiety during medical procedures. | |
What is New: • Our study found that with a small change in communication technique (called therapeutic communication or TC), the comfort of children during venipuncture improves. • This improved comfort was mainly reflected by reduced anxiety scores and shorter procedural time. This makes TC suitable for the outpatient setting. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Many children feel anxious when they need to undergo a medical examination or intervention. In particular, needle related procedures cause anxiety and fear in children [1,2,3,4,5,6]. This leads to more pain and emotional distress [2,3,4,5,6]. Failure to adequately manage pain and anxiety may have immediate negative consequences such as unsuccessful medical procedures and lack of cooperation from a child, leading to increased procedural time and adverse physiological reactions [3, 4, 6]. More far-reaching effects are increased pain perception, diminished analgesic effectiveness with subsequent procedures, and avoidance of medical care, which may persist into adulthood [4, 6]. Besides negatively impacting the child, significant child pain and anxiety during needle procedures can be highly distressing and challenging for parents and healthcare providers as well [7, 8].
In adults, the use of communication techniques based on hypnosis can be used to reduce pain and anxiety [9, 10]. These methods are based on establishing instant rapport, avoiding negative suggestions and reframing using a script or guided imagination. These techniques can be integrated in everyday patient interaction and as a supplement on procedural sedation or perioperative care [9,10,11]. Non-pharmacological psychological interventions for pain have also been investigated in children in the review of Birnie [2]. Distraction, breathing, hypnosis and combined cognitive and behavioral strategies can reduce pain and distress during needle procedures. The results of this review, however, should be interpreted with caution due to lack of blinding of patients and of outcome assessors [2]. To further examine the effects of communication techniques on procedural pain and comfort in children, more research is warranted.
Children experience medical procedures within the context of their family [12]. This means that a child’s coping strategy and its expectations are related to that of its parents [12]. So, when examining the effects of an intervention on pain and distress of the child, it is of importance to also assess the parent experience of this intervention (e.g., by measuring proxy pain, and self-reported and observed anxiety). Several studies have addressed the influence of parental anxiety on the child’s pain experience [13,14,15,16]. For example, one of the studies showed that parent (pre)procedural anxiety increases the child’s anxiety during the procedure which ultimately caused more child’s pain [13]. Therefore, in this study we will investigate the influence of parental anxiety on the child’s pain experience.
This study assesses the effects of therapeutic communication (TC) versus standard communication (SC). TC is based on Comfort Talk®, the LAURS of hypnotic communication and the ''Lived in Imagination'' Technique in an outpatient setting [9,10,11, 17, 18]. The objective of this study is to examine whether patient-centric TC positively affects children’s comfort during venipuncture. The primary outcome of this study is self-reported pain by children. Secondary outcomes are observed pain (child and parent), anxiety (child and parent), satisfaction (child, parents and medical personnel) and procedural time. Also, a mediation analysis will be conducted to investigate whether parents’ anxiety increases children’s pain through children’s anxiety. Finally, a subgroup analysis will be performed to investigate if TC is effective in neurodivergent children (e.g., with attention-deficit-hyperactivity-disorder (ADHD) or with autism spectrum disorder (ASD). This, to gain more insight in this topic as a considerable amount of children in our tertiary hospital is neurodivergent and there is lack of empiric evidence on patient comfort and venipuncture in these patients [19].
Methods and materials
Study design
After ethical approval (Ethics Committee CMO Arnhem-Nijmegen, Number 2019-5488), this single-blinded intervention study was performed in an outpatient clinic in a tertiary care hospital in Nijmegen, the Netherlands. The study was registered in the Dutch Trial Register (NL8221). Data was collected between January 2020 and October 2020.
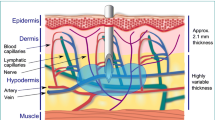
Participants
Children who needed to undergo venipuncture at the outpatient clinic were asked to participate in this study. Inclusion criteria were age between 5 and 18 years, use of topical anesthesia on the presumed needle insertion site (EMLA, Aspen, The Netherlands), and the ability to communicate in Dutch language by child and parent or guardian. Written informed consent was obtained prior to the study. For children in the age of 5 to 12 years or children with intellectual disabilities, informed consent was provided by parent or guardian. For children aged 12 to 16 years, it was provided by the child and parent or guardian, and for children up to and including 16 years, it was provided by the child.
Procedure
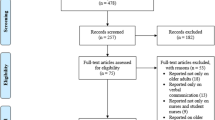
The study consisted of two groups that were subsequently studied: a SC group and a TC group. The SC group was studied in January and February 2020, and the TC group in September and October 2020. For the SC group, blood sampling procedures were performed according to standardized protocol and baseline data were obtained. After having included 51 patients, all personnel was trained in patient-centered TC. The training consisted of an eight-hours classroom session in which theoretical lectures about the scientific background were interchanged with practical demonstrations, exercises, and role-playing. Medical personnel was trained in how to establish quick empathic contact by matching nonverbal and verbal behavior, avoidance of negative verbal suggestions, the use of hypnotic language and expression of positive expectations (Supplementary Table 1: an overview of therapeutic communication techniques applied in our study). In August 2020, a four-hours refresher course was organized because of an interruption due to COVID-19. The TC group ended in October 2020 when 54 children were included (Fig. 1).
Measures
Demographic data
Demographic data was obtained prior to venipuncture (e.g. age, gender, underlying disease, amount of previous venipunctures and the presence of neurodivergent disorders (e.g. ADHD, ASD). To measure anxiety the child’s trait level of anxiety and the parents’ trait and state level of anxiety were obtained by the Spielberger State-Trait Anxiety questionnaire for children (STAI-C) and the Dutch version of the State-Trait Anxiety Inventory (STAI-Y), named ZBV for the parents [20].
Primary outcome measure
Self-reported pain
Self-reported pain was measured directly after venipuncture with the Faces Pain Scale-Revised (FPS-R) [21]. The FPS-R has been recommended for use following procedure-related pain in clinical trials for children of four years and older [21,22,23].
Secondary outcome measures
Observed pain
Directly after the venipuncture parents or guardians and medical professionals scored the observed pain of the child on a NRS (Numeric Rating Scale; 0 = no pain, 10 = worst pain ever).
Anxiety during venipuncture
Children 8 years or older reported their anxiety levels during venipuncture on a NRS (0 = no anxiety, 10 = worst anxiety ever). Parents or guardians and medical professionals scored the observed anxiety of the child and anxiety of the parent on the same NRS.
Satisfaction
Children 8 years or older, their parents or guardians and medical personnel reported their satisfaction about the procedure on a NRS (0 = unsatisfied, 10 = very satisfied).
Procedural time
The time the child spent in the room during venipuncture was measured in minutes.
Statistical analysis
For data analysis, IBM SPSS Statistics 26 was used. A power analysis was performed to determine the sample size that was needed to provide a 95% probability of detecting differences between groups. One face (i.e., 2 points, translating to an effect size of d = 0.8) on the FPS-R scale was assumed to be a clinically significant difference as proposed by Tsze et al. for the 7-point Faces Pain Scale [24]. The sample size was calculated with G*Power 3.1 and the required number to include was 42 in the SC group and 42 in the TC group in order to detect a statistically significant difference (p < 0.05).
Baseline group differences for demographic characteristics were determined with independent sample t-tests for continuous outcomes (age and anxiety) and with Chi-square tests for categorical outcomes (sex, psychiatric disorder, involvement of child life specialist, amount of venipunctures, use of calming medication).
To answer the primary research aim, namely to assess whether self-reported pain was lower after TC than SC, an independent sample t-test was performed to compare self-reported pain between the SC and the TC group. For the secondary aim of this study, namely to detect group differences between the SC and TC group for observed pain scores (by researcher, parent and medical personnel), anxiety scores (of the child and parent), satisfaction scores (of the child, parents and medical personnel), and time in the room, independent sample t-tests were performed. To answer the third research question, two mediation analyses were conducted for both groups to investigate whether parent procedural anxiety influences child procedural anxiety, which in turn, affects child’s procedural pain. Both analyses included parent self-reported procedural anxiety, child-reported procedural anxiety, and child-reported procedural pain. The Preacher and Hayes mediation macro was used to estimate indirect effects [25]. Finally, a subgroup analysis of neurodivergent children was performed with two-way analysis of variance (ANOVA), to investigate a possible interaction effect on anxiety between the of SC or TC group and having an ADHD/ASD diagnosis.
Results
Sample characteristics
In total, 105 children (range 5–17 years old) participated in the study. Demographic data are described in Table 1.
There were no differences in sample characteristics between the SC and TC group. Anxiety levels (measured with the STAI trait) did not differ between the SC and TC group. Outcome measures for the statistical analyses were checked for corresponding assumptions. Data of self-reported and observed pain scores were not normally distributed, and were therefore also analyzed with non-parametric tests (Mann–Whitney U test). Because this yielded no difference in results, all outcomes reported below are from parametric tests (independent sample t-tests, two-way ANOVA and regression analysis). See Table 2 for an overview of outcomes of group comparisons.
Primary outcome measure
Self-reported pain by children
There was no difference in self-reported pain by children between the TC group (M = 1.7, SD = 2.2) and SC group (M = 1.7, SD = 2.6), t(103) = 0.42, p = .967 (Fig. 2).
Secondary outcome measures
Observed pain
NRS pain scores observed by parents and by medical personnel did not significantly differ between the TC and SC group (Table 2).
Anxiety during venipuncture
For anxiety scores scored by the child, we found that children in the therapeutic communication group reported lower anxiety t(69) = 2.05, p = 0.45. For the other anxiety outcomes, we found that anxiety scores of the child were significantly lower in the TC group when scored by the parent t(103) = 2.36, p = .020, and by medical personnel t(103) = 2.47, p = .015. Anxiety scores of the parent were lower in the TC group when scored by the parents themselves t(103) = 2.55, p = .013, but not when scored by medical personnel (Fig. 3).
Satisfaction
There were no group differences in satisfaction for parents and children (Table 2). Medical personnel reported that they were more satisfied after TC than after SC t(102) = 2.65, p = 0.009 (Fig. 4).
Procedural time
Procedural time in the TC group was shorter (6min0s) than in the SC group (8min36s), t(103) = 2.53, p = .014 (Fig. 5).
Mediation analyses
Two mediation analyses were conducted to test the direct effect (parental procedural anxiety on child pain) and indirect effects (parental procedural anxiety on child pain via child anxiety) for the TC group and the SC group. The regression models were significant for the SC group (F(2,35) = 3.30, p = 0.048, R2 = 0.16) and the TC group (F(2,52) = 13.55, p < 0.001, R2 = 0.35). Based on the presence of zero in the confidence intervals for indirect paths, both analyses indicated no mediation effect of parental procedural anxiety on child pain via child anxiety (Fig. 6).
Subgroup analysis neurodivergence
Based on the significant outcome of child anxiety, the subgroup analysis was performed with anxiety as outcome. There were no differential effects of TC on anxiety for neurodivergent children versus non-neurodivergent children (i.e., no diagnosis of a psychiatric disorder), F(2,70) = .52, p = 0.596, ηp2 = .015).
Discussion
The objective of this study was to examine whether patient-centric TC positively affects children’s comfort during venipuncture. Comfort is defined as a ''transient and dynamic state characterized by ease from pain, emotional and physical distress and an emerging sense of positivity, safety, strength and acceptance of one’s situation that is underpinned and sustained by feeling valued, cared for, confident and accepting treatment. Patients seek to be as comfortable as they can be, under the circumstances of their healthcare interaction'' [26]. When assessing patient’s experience during interventional procedures the word comfort avoids the nocebo effect of the word pain. Unfortunately comfort scores correlate only moderately with pain scores [27]. Pain intensity and distress are considered primary outcomes for evaluating psychological interventions for needle-related procedures in children [2]. Pain and fear are positively associated with each other. Fear can increase the pain experience and fear can increase during acute pain [28]. The interdependence of these two variables made it difficult to decide which primary outcome should be defined. Because of the familiarity and routine measurement of pain scores in children in our hospital, we choose pain intensity as primary outcome measure.
No difference in self-reported pain was found between the SC and the TC group. For the secondary outcomes, however, scores significantly improved for anxiety, time in the room and satisfaction of the medical personnel. For the third research question, namely whether parental anxiety influences the child’s pain via the child’s anxiety, no mediation effect was found. For the fourth research question, we found that TC had the same effect on anxiety as in non-neurodivergent children.
The absence of significant self-reported pain results may be attributed to the overall low pain scores (95% CI [1.1, 2.4]), and these low pain scores did not indicate clinically relevant pain according to the optimal cut points for the FPS-R [29]. The low pain scores are probably the result of the use of EMLA which is an effective local anesthetic for pediatric venipuncture pain [30, 31]. This was implemented as standard procedure prior to venipuncture in our hospital. Literature varies on the effect of therapeutic communication/distraction techniques on pain, because these studies are difficult to compare as they differ in the use of EMLA, distraction technique, patient population and pain scores during venipuncture [10, 32,33,34].
All anxiety scores for the child (scored by child 8 years or older), parent and medical personnel) were lower in the TC group than in the SC group. The parents also scored lower self-reported NRS anxiety scores when TC was used. NRS anxiety for the parent scored by the medical personnel did not differ significantly between groups. Moreover, this study investigated the influence of parental anxiety on the relationship between the child’s anxiety and pain experience. No mediation effects were found (parental procedural anxiety on child pain via child anxiety) in both groups. This is in contrast with the study results of Bearden et al. (2012) where a mediation effect was found of preprocedural anxiety and procedural pain of the child, which in turn heightened the child’s pain [13]. This, again, may be due to the lack of higher pain scores in the current study. For satisfaction, this study found higher satisfaction for medical personnel in the TC group. We hypothesize that this higher satisfaction of the medical personnel was explained by more communication tools of the personnel to deal with anxious patients and their parents, which resulted in less delay and less stressful situations. Furthermore the personnel mentioned a better team climate and improved interaction between care givers themselves. However not investigated thoroughly in our study, this improved job satisfaction and better team climate was also described in other studies [11, 35]. The shorter procedural time and no need for other resources makes this communication technique very suitable for application in the outpatient clinic and at the emergency department.
Finally, because a large proportion of patient undergoing venipuncture is neurodivergent (28.6% in our sample), and because of the limited research conducted on this topic, we performed a subgroup analysis to find out if TC was also effective in the neurodivergent children (e.g., with ASD or ADHD) in our study. The results showed similar effects in anxiety reduction for neurodivergent children as non-neurodivergent children. However, this result must be interpreted with caution, as this analysis was exploratory and the sample of the subgroup analysis was relatively small (n = 30).
One of the strengths of this study was that when examining comfort during venipuncture, this study captured the multi-faceted context of this procedure. Different outcomes were measured (e.g., pain, anxiety, and satisfaction) from different perspectives (children, parents and medical personnel) thereby adopting an overall integrative approach. Moreover, this study aimed to contribute to the scarce literature of venipuncture comfort for neurodivergent children. However, adopting this integrative approach induces bias. Given the large amount of outcome measures, the likelihood of incorrectly rejecting a null hypothesis (i.e., making a Type I error) increases [36]. Furthermore, we recommend more emphasis on (neuro)divergent groups in future research, especially for children with ASD as these children often show higher levels of anxiety [19, 37,38,39].
To conclude, our study found that with just a small change in communication style, the comfort of the child during venipuncture improves. This was mainly reflected by reduced anxiety scores and shorter procedural times, making the use of TC during venipuncture promising for the outpatient setting.
Abbreviations
- ADHD:
-
Attention deficit hyperactivity disorder
- ANOVA:
-
Analysis of variance
- ASD:
-
Autism spectrum disorder
- EMLA:
-
Eutectic mixture of local anesthetics
- FPS-R:
-
Faces pain scale-revised
- NRS:
-
Numeric rating scale
- SC:
-
Standard communication
- STAI-C:
-
State trait anxiety inventory for children
- STAI-Y:
-
State trait anxiety inventory for adults (form Y)
- TC:
-
Therapeutic communication
- ZBV:
-
Zelf beoordelingsvragenlijst (ENG: self-report questionnaire)
References
Dalley JS, Morrongiello BA, McMurtry CM (2021) Children’s Perspectives on Outpatient Physician Visits: Capturing a Missing Voice in Patient-Centered Care. Children 8:1–15. https://doi.org/10.3390/children8010034
Birnie KA, Noel M, Chambers CT, Uman LS, Parker JA (2018) Psychological interventions for needle-related procedural pain and distress in children and adolescents. Cochrane Database Syst Rev 10:1–165. https://doi.org/10.1002/14651858.CD005179.pub4
McLenon J, Rogers MA (2019) The fear of needles: A systematic review and meta-analysis. J Adv Nurs 75:30–42. https://doi.org/10.1111/jan.13818
McMurtry CM, Riddell RP, Taddio A, Racine N, Asmundson GJ, Noel M, Chambers CT, Psych R, Shah V, HelpinKids&Adults Team (2015) Far From "Just a Poke": Common Painful Needle Procedures and the Development of Needle Fear. Clin J Pain 32:S3-S11. https://doi.org/10.1097/AJP.0000000000000272
Dumoulin S, Bouchard S, Ellis J, Lavoie KL, Vézina M-P, Charbonneau P, Tardif J, Hajjar A (2019) A randomized controlled trial on the use of virtual reality for needle-related procedures in children and adolescents in the emergency department. Games Healt J 8:285–293. https://doi.org/10.1089/g4h.2018.0111
Walco GA (2008) Needle pain in children: contextual factors. Pediatrics 122:S125-129. https://doi.org/10.1542/peds.2008-1055d
Kennedy RM, Luhmann J, Zempsky WT (2008) Clinical implications of unmanaged needle-insertion pain and distress in children. Pediatrics 122:S130–S133. https://doi.org/10.1542/peds.2008-1055e
Smith RW, Shah V, Goldman RD, Taddio A (2007) Caregivers’ responses to pain in their children in the emergency department. Arch Pediatr Adolesc Med 161:578–582. https://doi.org/10.1001/archpedi.161.6.578
Cyna AM (2019) The Laurs of Hypnotic Communication and the “Lived in Imagination” Technique in Medical Practice. Int J Clin Exp Hypn 67:247–261. https://doi.org/10.1080/00207144.2019.1612669
Lang EV, Berbaum KS, Faintuch S, Hatsiopoulou O, Halsey N, Li X, Berbaum ML, Laser E, Baum J (2006) Adjunctive self-hypnotic relaxation for outpatient medical procedures: a prospective randomized trial with women undergoing large core breast biopsy. Pain 126:155–164. https://doi.org/10.1016/j.pain.2006.06.035
Lang EV (2012) A better patient experience through better communication. J Radiol Nurs 31:114–119. https://doi.org/10.1016/j.jradnu.2012.08.001
Bowen M (1966) The use of family theory in clinical practice. Compr Psychiatry 7:345–374. https://doi.org/10.1016/s0010-440x(66)80065-2
Bearden DJ, Feinstein A, Cohen LL (2012) The influence of parent preprocedural anxiety on child procedural pain: mediation by child procedural anxiety. J Pediatr Psychol 37:680–686. https://doi.org/10.1093/jpepsy/jss041
Bernard RS, Cohen LL (2006) Parent anxiety and infant pain during pediatric immunizations. J Clin Psychol Med Settings 13:282–287. https://doi.org/10.1007/s10880-006-9027-6
Lipani TA, Walker LS (2006) Children’s appraisal and coping with pain: Relation to maternal ratings of worry and restriction in family activities. J Ped Psychol 31:667–673. https://doi.org/10.1093/jpepsy/jsj038
Whaley SE, Pinto A, Sigman M (1999) Characterizing interactions between anxious mothers and their children. J Consult Clin Psychol 67:826–836. https://doi.org/10.1037//0022-006x.67.6.826
Lang EV, Viegas J, Bleeker C, Bruhn J, van Geffen G-J (2017) Helping children cope with medical tests and interventions. J Radiol Nurs 36:44–50. https://doi.org/10.1016/j.jradnu.2016.11.005
Cyna AM (2020) Little words BIG impact: Perioperative communication for children with burns. Anaesth Intensive Care 48:123–128. https://doi.org/10.1177/0310057X20914909
Davit CJ, Hundley RJ, Bacic JD, Hanson EM (2011) A pilot study to improve venipuncture compliance in children and adolescents with autism spectrum disorders. J Dev Behav Pediatr 32:521–525. https://doi.org/10.1097/DBP.0b013e3182245b09
Van der Ploeg HM, Defares PB, Spielberger CD (1980) Handleiding bij de Zelf-Analyse Vragenlijst, ZAV [Manual for the Self-Analysis Questionnaire, ZAV]
Hicks CL, von Baeyer CL, Spafford PA, van Korlaar I, Goodenough B (2001) The Faces Pain Scale–Revised: toward a common metric in pediatric pain measurement. Pain 93–173–183. https://doi.org/10.1016/S0304-3959(01)00314-1
McGrath PJ, Walco GA, Turk DC, Dworkin RH, Brown MT, Davidson K, Eccleston C, Finley A, Goldschneider K, Haverkos, et al (2008) Core outcome domains and measures for pediatric acute and chronic/recurrent pain clinical trials: PedIMMPACT recommendations. J Pain 9:771–783. https://doi.org/10.1016/j.jpain.2008.04.007
Tomlinson D, von Baeyer CL, Stinson JN, Sung L (2010) A systematic review of faces scales for the self-report of pain intensity in children. Pediatrics 126:e1168–e1198. https://doi.org/10.1542/peds.2010-1609
Tsze DS, Hirschfeld G, Dayan PS, Bulloch B, von Baeyer CL (2018) Defining no pain, mild, moderate, and severe pain based on the Faces Pain Scale-Revised and Color Analog Scale in children with acute pain. Pediatr Emerg Care 34:537–544. https://doi.org/10.1097/PEC.0000000000000791
Preacher KJ, Hayes AF (2004) SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav Res Methods 36:717–731. https://doi.org/10.3758/bf03206553
Wensley C, Botti M, McKillop A, Merry AF (2020) Maximising comfort: how do patients describe the care that matters? A two-stage qualitative descriptive study to develop a quality improvement framework for comfort-related care in inpatient settings. BMJ Open 10:1–18. https://doi.org/10.1136/bmjopen-2019-033336
Miu MW, Martin A, Cyna AM. Postoperative pain and comfort scores: Do they correlate? Anaesthes Intensive Care 47:435–441. https://doi.org/10.1177/0310057X19861985
Hedén L, von Essen L, Ljungman G (2019) Children’s self-reports of fear and pain levels during needle procedures. Nurs Open 7:376–382. https://doi.org/10.1002/nop2.399
Tsze DS, Hirschfeld G, von Baeyer CL, Bulloch B, Dayan PS (2015) Clinically significant differences in acute pain measured on self-report pain scales in children. Acad Emerg Med 22:415–422. https://doi.org/10.1111/acem.12620
Rogers TL, Ostrow CL (2004) The use of EMLA cream to decrease venipuncture pain in children. J Pediatr Nurs 19:33–39. https://doi.org/10.1016/j.pedn.2003.09.005
Tak J, Van Bon W (2006) Pain-and distress-reducing interventions for venepuncture in children. Child Care Health Dev 32:257–268. https://doi.org/10.1111/j.1365-2214.2006.00578.x
Fanurik D, Koh JL, Schmitz ML (2000) Distraction techniques combined with EMLA: Effects on IV insertion pain and distress in children. Child Health Care 29:87–101. https://doi.org/10.1207/S15326888CHC2902_2
Fusco N, Bernard F, Roelants F, Watremez C, Musellec H, Laviolle B, Beloeil H (2020) Hypnosis and communication reduce pain and anxiety in peripheral intravenous cannulation: Effect of Language and Confusion on Pain During Peripheral Intravenous Catheterization (KTHYPE), a multicentre randomised trial. Br J Anaesth 124:292–298. https://doi.org/10.1016/j.bja.2019.11.020
Liossi C, White P, Hatira P (2009) A randomized clinical trial of a brief hypnosis intervention to control venepuncture-related pain of paediatric cancer patients. Pain 14:255–263. https://doi.org/10.1016/j.pain.2009.01.017
Ajam AA, Tahir A, Makary MS, Longworth S, Lang EV, Krishna NG, Mayr NA, Nguen XV (2020) Communication and team interactions to improve patient experiences, quality of care, and throughput in MRI. Top Magn Reson Imaging 29:131–134. https://doi.org/10.1097/RMR.0000000000000242
Mittelhammer RC, Judge GG, Miller DJ (2000) Econometric foundations pack with CD-ROM. Cambridge University Press, Cambridge
Evans DW, Canavera K, Maccubbin E, Taga K (2005) The fears, phobias and anxieties of children with autism spectrum disorders and down syndrome: Comparisons with developmentally and chronologically age matched children. Child Psychiatry Hum Dev 36:3–26. https://doi.org/10.1007/s10578-004-3619-x
MacNeil BM, Lopes VA, Minnes PM (2009) Anxiety in children and adolescents with autism spectrum disorders. Res Autism Spectr Disord 3:1–21. https://doi.org/10.1016/j.rasd.2008.06.001
White SW, Oswald D, Ollendick T, Scahill L (2009) Anxiety in children and adolescents with autism spectrum disorders. Clin Psych Rev 29:216–229. https://doi.org/10.1016/j.cpr.2009.01.003
Funding
Author R.M.S. has received research support from the National Health Care Institute (2017045964).
Author information
Authors and Affiliations
Contributions
LAMA and GJvG contributed to the conception and design of the study. Data collection was performed by LAMA and EV. Data analysis was carried out by RMS. The first draft of the manuscript was written by LAMA and RMS and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the medical ethical committee CMO region Arnhem-Nijmegen (May 24, 2019/N0 2019-5488).
Consent to participate
Informed consent was obtained from all individual participants included in the study
Consent to publish
The authors affirm that human research participants provided informed consent for publication
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Storage of data
Subject, code and patient identification were saved in an identification log. A key file with password for the identifying personal data, linked to the study code, was saved on a separate file and was only accessible for the researchers. On the Case Report Form and in the database (Castor EDC) only coded data was used, no personal identification data. Data was saved for 15 years.
Additional information
Communicated by Piet Leroy.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Aarts, L.A.M., van Geffen, GJ., Smedema, E.A.L. et al. Therapeutic communication improves patient comfort during venipuncture in children: a single-blinded intervention study. Eur J Pediatr 182, 3871–3881 (2023). https://doi.org/10.1007/s00431-023-05036-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-05036-7